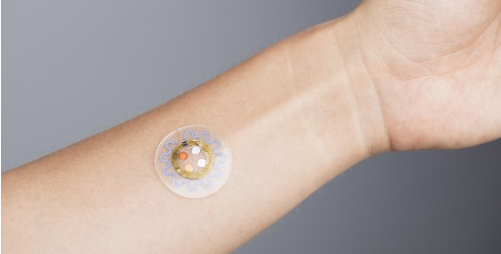
Sweat may be smelly and annoying, but it also offers potentially useful insights into our health. Inspired by wearable devices like the Fitbit, researchers are now designing small flexible patches, similar to Band-Aids, which can analyze the chemical composition of our sweat.
While fitness wristbands can measure heart-rate, number of steps, and distance (with less than perfect accuracy), a sweat tracker can go even further, helping diabetics track their glucose levels, warning athletes and soldiers when they’re getting dehydrated, and letting drinkers know when it’s time to stop. Researchers say there are over 100 different variables that can be traced in sweat.
“I look at sweat as a sort of diluted version of blood,” says Tolga Kaya, an associate professor of electronics engineering at Central Michigan University, “whatever you see in your blood, most of it will be in your sweat as well.”
Traditionally, measuring glucose, electrolytes, or hormones in the body has meant drawing blood, often followed by days or weeks of laboratory analysis. An additional drawback of blood tests is that they represent a static measurement taken at a single point in time. Unlike sweat measurements, blood does not offer the ability to monitor continuous changes in health. Conventional blood tests not only delay results, but they can also be painful and inconvenient. The hope is that sweat analysis could offer a quicker, continuous, and pain-free alternative.
Although nearly everyone would prefer a Band-Aid to a blood test, concentrations of biological chemicals are much smaller in sweat than in blood – so it’s challenging to design a skin patch that can measure these substances accurately.
Currently, there are very few sweat measurements accurate enough to use for clinical diagnosis. The stress hormone cortisol’s sweat-to-blood correlation is well-established, and measuring salt concentration in sweat is considered the gold standard for diagnosing cystic fibrosis. However, for other chemical substances, most new research is aimed at ensuring sweat measurements correctly translate to blood measurements.
While challenges in translating blood to sweat measurements persist, diabetes remains an obvious target for sweat trackers. Today, insulin-dependent type 1 and type 2 diabetics have to prick their fingers several times a day to read out their glucose levels and decide whether they need to stabilize their blood sugar.
Researchers at the University of Texas at Dallas are testing a wearable patch that would avoid the need for such finger pricks. Their sensor is capable of measuring glucose in just a microliter of sweat – a quantity about the size of a single grain of salt.
In a July 2016 study, the researchers compared measurements from their non-invasive sweat glucose monitor to a TrueResult blood glucose monitor and found a 95 percent correlation between the readings. By research standards, this means the sweat monitor “passed the test” and is a positive step toward further increasing the accuracy of this type of biosensor.
A prototype of this device could be available for consumers in 12-18 months. It is important to note that making the device completely accurate is still a work in progress. “It will help you monitor your glucose levels,” says Shalini Prasad, a biomedical researcher and co-author of this study. “But if you want a clinical diagnosis, you would still need to rely on the blood glucose measurements until that official correlation gets established.”
Sweat-sensing wearable devices could also monitor dehydration states in athletes and soldiers. Kaya and his colleagues at the University of California recently developed a sensor that measures the rate of sweat as well as its electrolyte content. Both of these measurements are indicators of dehydration. Previously, Kaya also worked on patches that measure lactate levels which reflect fatigue during exercise.
The advantage of using sweat measurements in this instance is that the sweat patch can collect and monitor changes continuously and deliver real time results. The user could monitor changes in their hydration state minute by minute. With blood, this type of monitoring would be impossible.
Kaya envisions applying this technology to high performance athletes. He refers to the example of an NBA final, in the 7th game and the 4th quarter. As the coach is making the decision of who should take the shot, there are many things to consider.
“One of the important things is that we know that dehydration is not just a physical state, but also a mental state,” says Kaya, “when someone is dehydrated, they cannot make important decisions… By monitoring an athlete’s dehydration state all the time, we can keep them in peak performance.”
Kaya also hopes to see soldiers using this type of technology on the battlefield. While on duty, the physical and mental states of soldiers are key to their survival. Soldiers could monitor their sweat composition in real time and use the information to alter their water or food intake to remain healthy and alert.
Sweat sensors are also in development to measure blood alcohol levels. Other than drawing blood, most methods to measure blood alcohol levels, including breathalyzers, are prone to inaccuracies.
Researchers at the University of California San Diego created a device that can detect alcohol levels in sweat, and then send that information via Bluetooth to the user’s cell phone. Ideally, these sensors would discourage individuals from drinking in excess and deter them from driving drunk.
The accuracy of these alcohol sensors is still in development – as is the way the user might receive and use the information. “Now we are improving smartphone applications to make them more user-friendly,” says Jayoung Kim, the lead graduate student involved in this study. “For example, it could send an alarm to your friends or call an Uber if you drink too much at a party.”
While the applications for sweat analysis seem endless, we are still a ways off from replacing blood tests – much less doctors – with a Band-Aid-sized skin patch. Sweat contains many, but not all of the components found in blood. A complete blood cell count, which indicates conditions such as anemia, infection, or certain cancers, are measurements that are impossible with sweat. However, as research continues to grow in this field, sweat may become a widely-used alternative for certain clinical diagnostics. Rather than seeing sweat as a nuisance we need to control, perhaps it’s time to see it as a tool to keep us informed about our health.


[…] zie zweet als een soort verdunde versie van bloed”, aldus Tolga Kaya, onderzoeker van Cental Michigan University. “Wat je in je bloed ziet, zie je […]